Diabetes is a chronic condition that affects millions of people worldwide. It's caused by the body's inability to produce or use insulin, a hormone that regulates blood sugar levels. While most people are aware of the common symptoms of diabetes, such as frequent urination, excessive thirst, and fatigue, many don't know that the condition can also manifest on the skin. In fact, the skin is often a reflection of what's going on inside the body. This article will examine certain indications that could emerge on your skin as a warning if you have diabetes. By recognizing these signs, you can take action to manage your condition and prevent complications.
See Also: These Healthy Habits Are Not So Beneficial For Diabetes
1. Acanthosis Nigricans - Dark, Velvety, Tanned Skin

Image source: Wikimedia Commons
Have you ever noticed a tan or brown mark on your skin that just won't budge, no matter how much you scrub it? This frustrating condition is a common occurrence among people with diabetes, known as acanthosis nigricans (pronounced: ah-kan-THO-sis NY-gruh-kans). The condition causes the skin to thicken and darken, exhibiting a velvety texture that may lead to itchiness and an unpleasant smell. Acanthosis nigricans commonly appears on the back of the neck, groin, elbows, knees, knuckles, and armpits. People who are overweight or obese are more likely to develop acanthosis nigricans, making weight loss an effective treatment method. Recognizing this warning sign can help you take action and prevent further complications associated with diabetes.
2. Digital sclerosis - Hard, thickening skin
One of the lesser-known complications of diabetes is digital sclerosis, which initially presents as taut, thick, and wax-like skin on the fingers, leading to stiffness in the finger joints. When blood sugar levels remain uncontrolled, digital sclerosis can cause the skin to thicken, harden, and become swollen. This can spread to various parts of the body, including the upper back, arms, and shoulders. In some rare cases, thickened skin patches may appear over the knees, ankles, or elbows, making it challenging to move these joints. The texture of the thickened skin often resembles that of an orange peel.
Unfortunately, approximately one third of people with type 1 diabetes are affected by this condition, according to the American Diabetes Association. However, the good news is that by keeping blood sugar levels under control, people with diabetes can reduce their risk of developing complications associated with digital sclerosis and improve their overall health.
3. Diabetic dermopathy - Shin Spots
While many people may dismiss them as harmless age spots, those roundish, rough patches that commonly appear on the front of your legs, or shins, could actually be a sign of diabetes-related skin damage. These patches, known as dermopathy, are caused by high blood sugar levels that damage small blood vessels and result in brownish patches on the skin. Although they may not induce any pain, scratching, or exposed lesions, it's important to acknowledge them as a possible indication of diabetes.
In rare cases, dermopathy can appear in other areas of the body, such as the arms, thighs, and trunk. While the condition is typically harmless and fades away on its own within 18 months, it can also persist for a long time. Therefore, individuals who experience dermopathy should seek medical attention to manage their diabetes and prevent further complications.
4. Bullosis diabeticorum – Blisters
Although not a common symptom, diabetes can sometimes cause unexpected blistering on the skin. These blisters may vary in size, from one large blister to several smaller ones, and tend to appear on the hands, feet, legs, or forearms. The appearance of these blisters can be alarming as they resemble blisters that form after a severe burn. However, despite their appearance, they are typically painless and will heal on their own within approximately three weeks.
Maintaining healthy blood glucose levels is the only way to manage this skin problem associated with diabetes.
See Also: 12 Commonly Cited Diabetes "Facts" That Are Untrue
5. Necrobiosis Lipoidica- Yellow, reddish, or brown patches on the skin
Another lesser-known skin condition associated with diabetes is a red, raised area that appears similar to dermopathy but is larger, deeper, and spaced apart. Initially, it may seem dull and unremarkable, but as the condition progresses, it can become itchy, and painful, and develop into a shiny scar with visible blood vessels. This condition is quite rare, with only 1 in 300 diabetes patients experiencing it. Moreover, it is challenging to treat, and conventional treatments such as prescription medications, injections, or lotions may not always be effective.
The condition may also manifest in cycles, with active periods, followed by inactive ones, only to become active again. It can be difficult to manage due to this pattern, and patients may need to try several different treatment options before finding the one that is most effective. Furthermore, as with many skin conditions, early detection is crucial, and anyone experiencing unusual changes in their skin should seek medical advice promptly.
6. Eruptive Xanthomatosis - Outbreak of small, reddish-yellow bumps
Uncontrolled diabetes can lead to a condition known as eruptive xanthomatosis. This condition is characterized by pea-like, yellow skin growths surrounded by a red halo, which can be itchy. These bumps tend to appear on the hands, feet, arms, and buttocks, and while they may be tender, they are not contagious.
Eruptive xanthomatosis typically affects young men with high cholesterol and triglyceride levels. In addition to managing blood glucose levels, doctors may recommend reducing cholesterol and triglycerides through medication to manage this condition.
7. Bacterial infections
While bacterial skin infections can affect anyone, diabetics are at a greater risk due to high blood sugar levels that can lead to dry skin and a weakened immune system. Patients with diabetes often experience specific bacterial skin problems such as sties (red, painful lump near the edge of the eyelid that may look like a boil or pimple), nail infections, and deep carbuncles in the skin and surrounding tissue. These infections can result in redness, swelling, and painful sensations in the affected area. Seek medical attention if you experience any discomfort, itching, or inflammation on your skin, especially if you have high blood sugar or diabetes. Treatment usually involves antibiotic creams or pills, which can help manage and clear up these skin problems.
8. Fungal infections

Diabetic patients are at an increased risk of developing fungal infections, specifically Candida albicans. This fungus, which resembles yeast, can result in a red and irritating rash often accompanied by small blisters and scales. Typically, the rash occurs in damp and warm regions of the body such as beneath the breasts, between the toes, around the fingernails, or in the armpits. Other common fungal infections among diabetics include jock itch, athlete’s foot, ringworm, and vaginal yeast infections. It is recommended that you consult with your physician to determine the most effective medication for eliminating fungal skin issues.
9. Dry, itchy skin

It's not uncommon to experience dry and itchy skin, even if you're not living with diabetes. In many cases, inadequate blood flow, which is prevalent among diabetes patients, can be attributed to the underlying cause of this condition. If you find that your lower legs are particularly itchy, it could be due to inadequate blood flow. To alleviate this discomfort, you may want to reduce the frequency of your showers and use gentle soap when you do bathe. Additionally, applying moisturizing lotion to your skin can be helpful, but be sure to avoid putting it between your toes.
See Also: 7 Exercises That Are Effective for Controlling Diabetes
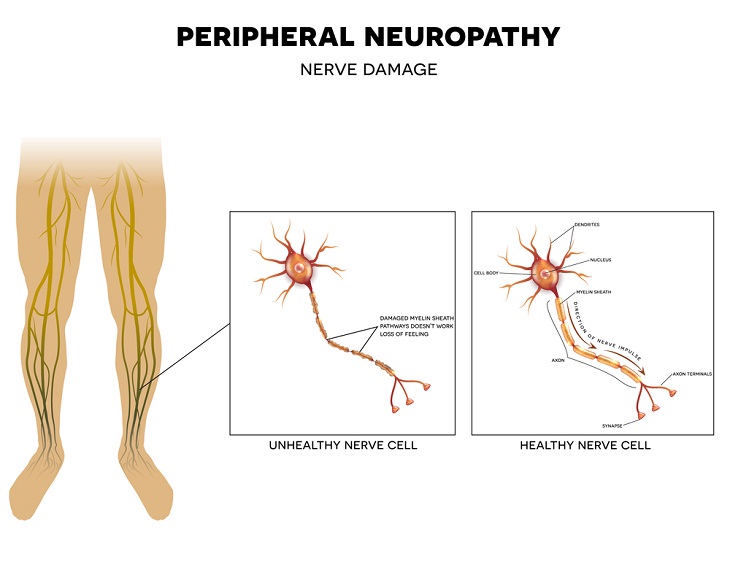
10. Peripheral Neuropathy - Damage to the nerves
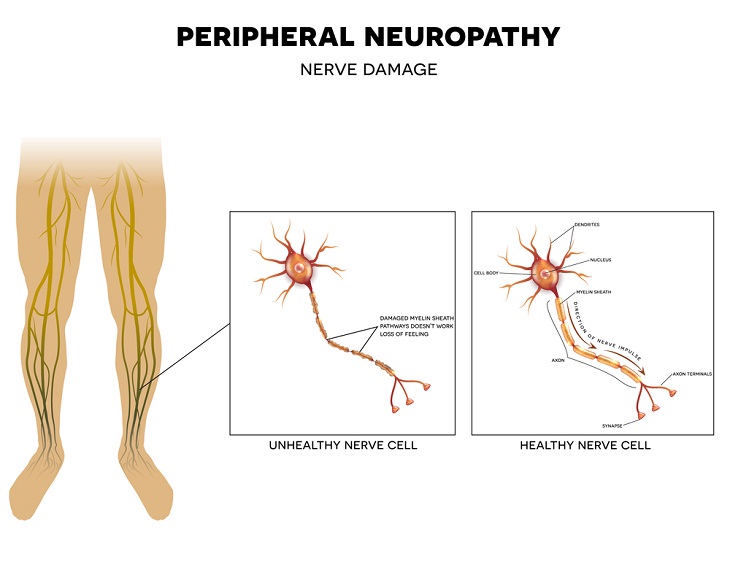
Diabetes can result in a type of nerve damage known as neuropathy, a common complication that involves damage to the nerves located outside of the brain and spinal cord. This can lead to a lack of sensation in the feet, making it difficult to detect injuries or blisters. In some cases, a foot ulcer may develop and become infected, posing a serious health risk. It's worth noting that while diabetes is a primary cause of neuropathy, there are other factors to consider, such as chemotherapy, autoimmune diseases, toxins, infections, and nutritional deficiencies. Make it a habit to examine your feet daily to ensure that they are not injured in any way.
 Go to BabaMail
Go to BabaMail